Are you curious about the potential of stem cell therapies to address age-related macular degeneration in Malaysia? In this article, we will explore the possibilities and advancements in stem cell research that may offer new hope for individuals suffering from this degenerative eye disease. With a focus on the Malaysian context, we will delve into the latest findings, potential treatments, and the impact these therapies could have on the lives of those affected. Join us as we uncover the potential of stem cell therapies in the fight against age-related macular degeneration in Malaysia.

Introduction
Age-related macular degeneration (AMD) is a progressive eye condition that affects millions of people worldwide. In Malaysia, the prevalence of AMD is a cause for concern, as it poses significant challenges to the healthcare system and impacts the quality of life for affected individuals. Traditional treatment options, such as medication and surgery, have limitations and do not provide a cure. However, there is growing potential in the field of stem cell therapies for addressing AMD and offering new hope for patients. This article will explore the potential of stem cell therapies in addressing AMD, advancements in stem cell research, challenges and limitations, clinical trials and research in Malaysia, international progress and success stories, and the future of stem cell therapies.
Understanding Age-related Macular Degeneration
Definition and Symptoms
Age-related macular degeneration (AMD) is a common eye condition that primarily affects older adults. It is characterized by the gradual deterioration of the macula, a small area in the center of the retina responsible for sharp, central vision. As a result, individuals with AMD experience a loss of central vision, which can significantly impact daily activities such as reading, driving, and recognizing faces.
The symptoms of AMD can vary from person to person, but they often include blurred or distorted vision, difficulty seeing in low light or at night, and a gradual loss of color vision. In the early stages, AMD may go unnoticed or cause minimal vision problems, but as the condition progresses, the impact on vision becomes more pronounced.
Prevalence in Malaysia
In Malaysia, AMD is a growing public health concern due to its increasing prevalence and the aging population. According to a study conducted by the National Eye Database (NED) in 2019, the prevalence of AMD in Malaysia was estimated to be 10.7% among individuals aged 50 and above. This translates to a significant number of individuals at risk of vision loss and the associated burdens on healthcare resources.
The high prevalence of AMD in Malaysia highlights the urgent need for effective treatment options that can halt or reverse the progression of the disease. Traditional treatment modalities, such as medication and surgery, have limitations and do not provide a complete solution. However, recent advancements in stem cell research offer new hope for addressing AMD and improving the lives of patients.

Current Treatment Options
Medication and Lifestyle Changes
Currently, the first-line treatment for AMD involves the use of medications, such as anti-vascular endothelial growth factor (anti-VEGF) drugs. These drugs help reduce abnormal blood vessel growth and leakage in the retina, which are key contributors to the progression of AMD. While these medications can slow down the progression of the disease and preserve vision to some extent, they require frequent injections into the eye and may not be suitable for all patients.
In addition to medication, lifestyle changes such as quitting smoking, eating a healthy diet rich in fruits and vegetables, maintaining a healthy weight, and protecting the eyes from UV radiation can also help reduce the risk of AMD or slow down its progression. However, these lifestyle changes may not be sufficient to address the underlying causes of AMD or reverse the damage already sustained by the macula.
Photodynamic Therapy
Another treatment option for certain types of AMD is photodynamic therapy (PDT). It involves the use of a light-activated drug that is injected into a vein and travels to the blood vessels in the eye. The drug is then activated by shining a laser light on the treated area, which causes damage to the abnormal blood vessels and helps slow down the progression of AMD. However, PDT is not suitable for all types of AMD and may have limited effectiveness in certain cases.
Intravitreal Injections
Intravitreal injections, also known as anti-VEGF injections, are commonly used to treat AMD. These injections deliver medication directly into the eye to inhibit the growth of abnormal blood vessels and reduce inflammation. While they can be effective in stabilizing or improving vision in some patients, they require regular administration and carry the risk of complications such as infection or retinal detachment. The need for repeated injections and the associated discomfort can also be burdensome for patients.
Implantable Telescope
For individuals with advanced AMD and significant vision loss, an implantable telescope may be an option. The telescope is surgically implanted into the eye and helps magnify central vision, allowing patients to see objects at a distance more clearly. However, this treatment option is limited to a select group of patients who meet specific criteria, and the procedure carries potential risks and complications.
Retinal Translocation Surgery
Retinal translocation surgery is a complex procedure that involves moving the macula to a healthier area of the retina to improve vision. It is typically reserved for individuals with advanced AMD who have a specific type of macular degeneration called subfoveal choroidal neovascularization (CNV). While this surgery can potentially restore some degree of vision, it is associated with significant risks, including retinal detachment and other complications.
Anti-VEGF Therapy
Anti-VEGF therapy, as mentioned earlier, involves the use of medications that target vascular endothelial growth factor (VEGF), a protein responsible for the abnormal blood vessel growth in the retina. These medications help reduce the leakage and bleeding associated with AMD, thereby slowing down its progression. While anti-VEGF therapy can be beneficial in managing the symptoms of AMD, it is not curative and requires ongoing treatment to maintain its effectiveness.
Despite these treatment options, there is still a need for more effective and long-lasting solutions for treating AMD. This is where stem cell therapies come into the picture, offering the potential to address the root causes of AMD and restore vision.
The Potential of Stem Cell Therapies
What are Stem Cells?
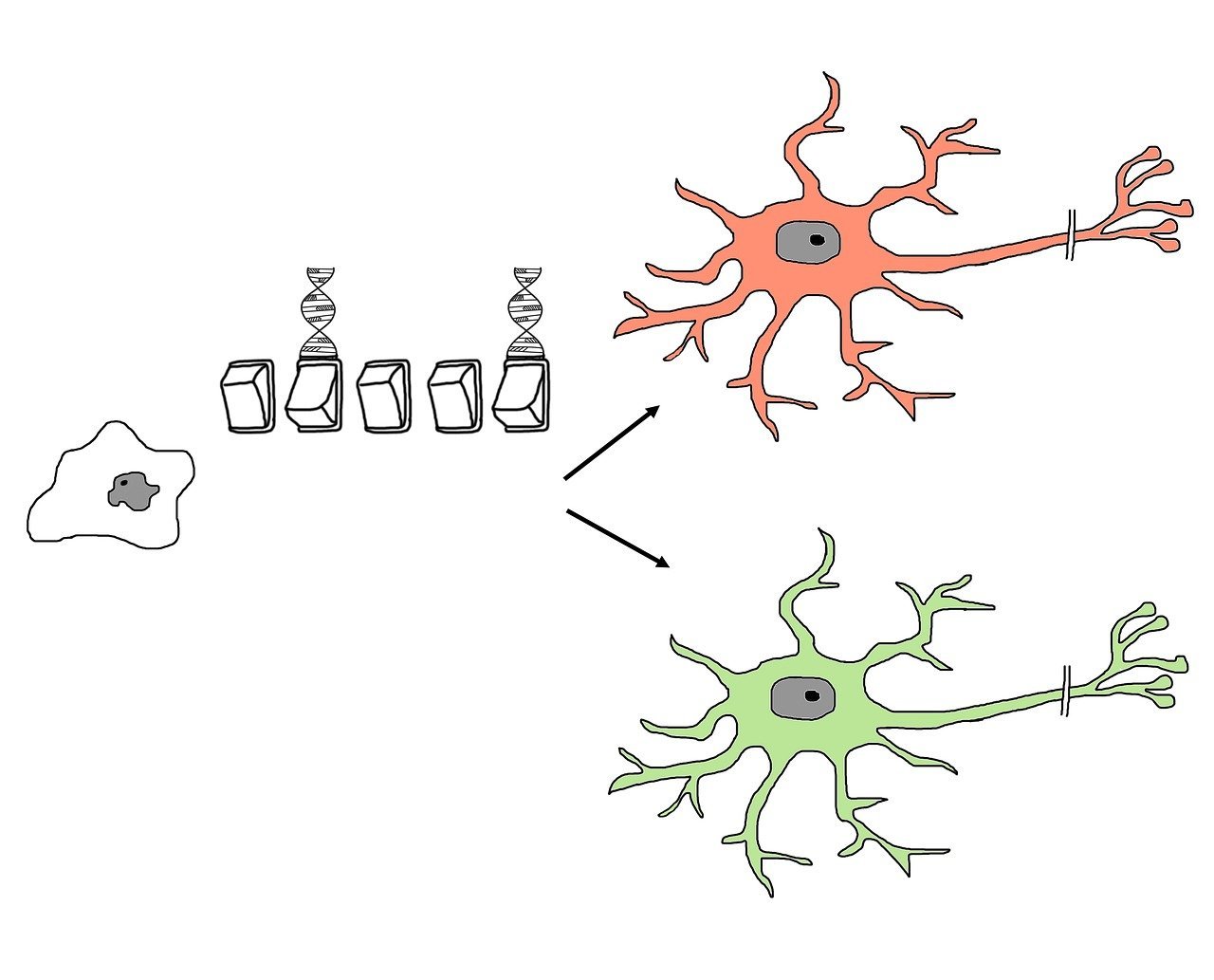
Stem cells are undifferentiated cells that have the remarkable ability to develop into different types of specialized cells in the body. They have the potential to regenerate and repair damaged tissues, making them a promising tool for treating a variety of diseases and conditions, including AMD.
In the context of AMD, stem cells can potentially differentiate into retinal cells and replace the damaged or degenerated cells in the macula. By restoring the structure and function of the retina, stem cell therapies offer a unique approach to addressing AMD at its core.
Types of Stem Cells used in Research
There are several types of stem cells that have been studied for their potential in treating AMD. These include induced pluripotent stem cells (iPSCs), embryonic stem cells (ESCs), and adult stem cells.
Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPSCs) are cells that have been reprogrammed from adult cells, such as skin cells, to exhibit pluripotent properties. Pluripotency means that these cells have the ability to differentiate into any cell type in the body, including retinal cells. iPSCs offer great potential for personalized medicine, as they can be derived from a patient’s own cells, minimizing the risk of rejection or immune response.
Embryonic Stem Cells
Embryonic stem cells (ESCs) are derived from the inner cell mass of a developing embryo. They are also pluripotent and have the ability to differentiate into various cell types, including retinal cells. ESCs have been extensively studied for their potential in regenerative medicine and have shown promising results in preclinical studies.
Adult Stem Cells
Adult stem cells, also known as tissue-specific or somatic stem cells, are found in various tissues and organs throughout the body, including the bone marrow, blood, and the eye. These stem cells have a more limited differentiation potential compared to pluripotent stem cells, but they can still contribute to tissue repair and regeneration.
In the context of AMD, adult stem cells derived from the eye itself or other sources, such as the bone marrow, have been investigated for their potential in promoting retinal repair and regeneration.
How Stem Cells can Address Macular Degeneration
The potential of stem cell therapies in addressing AMD lies in their ability to restore the damaged retinal tissue and promote the growth of healthy retinal cells. By introducing stem cells into the damaged macula, it is possible to stimulate the regeneration of retinal cells and restore their function.
Studies have shown that stem cells can differentiate into retinal pigment epithelial (RPE) cells, which play a crucial role in the health and function of the retina. RPE cells provide support to the photoreceptor cells in the macula, ensuring their proper function and protecting them from oxidative stress.
In AMD, the RPE cells become dysfunctional and fail to perform their protective role adequately. By replacing these damaged RPE cells with healthy ones derived from stem cells, it is possible to restore the health and function of the macula, thereby improving vision in individuals with AMD.

Advancements in Stem Cell Research
Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPSCs) have revolutionized the field of regenerative medicine by offering a personalized and potentially limitless source of stem cells for therapeutic use. iPSCs can be generated by reprogramming adult cells, such as skin cells, to exhibit pluripotent properties similar to embryonic stem cells.
Research has shown that iPSCs can differentiate into retinal cells, including RPE cells, and can be used to replace damaged or degenerated cells in the macula. This holds great promise for the development of personalized stem cell therapies for AMD, as iPSCs can be derived from a patient’s own cells, minimizing the risk of rejection or immune response.
Embryonic Stem Cells
Embryonic stem cells (ESCs) have long been considered a valuable tool in regenerative medicine due to their pluripotency and ability to differentiate into different cell types. ESCs can be derived from the inner cell mass of developing embryos and have been extensively studied for their potential in treating a variety of diseases and conditions, including AMD.
In the context of AMD, ESCs can be directed to differentiate into retinal cells, including RPE cells, and used to replace the damaged or dysfunctional cells in the macula. Preclinical studies have shown promising results, with ESC-derived RPE cells demonstrating the ability to integrate into the retinal tissue and improve visual function in animal models of AMD.
Adult Stem Cells
Adult stem cells, also known as tissue-specific or somatic stem cells, are present in various tissues and organs throughout the body, including the eye. These stem cells have a more limited differentiation potential compared to pluripotent stem cells, but they can still contribute to tissue repair and regeneration.
In the context of AMD, adult stem cells derived from the eye itself or other sources, such as the bone marrow, have been investigated for their potential in promoting retinal repair and regeneration. Research has shown that these stem cells can differentiate into RPE-like cells and have the ability to improve the structure and function of the macula.
Stem Cell Banking
Stem cell banking, also known as stem cell preservation or cryopreservation, involves the collection and storage of stem cells for future use. This practice allows individuals to preserve their own stem cells, either from various tissues or through the reprogramming of adult cells to iPSCs, for potential use in regenerative therapies.
Stem cell banking holds great potential for personalized medicine, as it allows individuals to store their stem cells while they are still young and healthy. These stored stem cells can then be used later in life, should the need arise, to treat diseases and conditions such as AMD.
Challenges and Limitations
Safety and Efficacy Concerns
One of the main challenges in stem cell therapies for AMD is ensuring their safety and efficacy. Stem cell therapies involve the transplantation of living cells into the eye, which carries the risk of complications such as infection, inflammation, and immune rejection. It is crucial to conduct thorough preclinical and clinical studies to assess the safety and effectiveness of stem cell therapies before they can be widely used in AMD patients.
Regulatory Framework
The field of stem cell therapies is still evolving, and there is a need for clear regulatory frameworks to govern their development and use. Regulatory bodies play a crucial role in assessing the safety and efficacy of new therapies and ensuring that they meet certain standards before being approved for clinical use.
In Malaysia, the National Pharmaceutical Regulatory Agency (NPRA) is responsible for regulating stem cell therapies and ensuring their safety, efficacy, and quality. The NPRA has developed guidelines and regulations to govern the development, clinical trials, and commercialization of stem cell therapies. However, there is a need for ongoing monitoring and updates to keep pace with the rapid advancements in the field.
Ethical Considerations
The use of certain types of stem cells, such as embryonic stem cells, raises ethical considerations due to their derivation from human embryos. In many countries, including Malaysia, there are restrictions and ethical guidelines in place for the use of embryonic stem cells in research and therapies.
However, advancements in reprogramming techniques, such as iPSCs, have provided an alternative source of pluripotent stem cells that does not involve the use of embryos. iPSCs offer the potential for personalized medicine and bypass many of the ethical concerns associated with the use of embryonic stem cells.
Cost and Accessibility
Stem cell therapies can be costly, especially in the early stages of development and implementation. The process of isolating, culturing, and differentiating stem cells can be expensive and requires specialized facilities and expertise. In addition, the clinical infrastructure, including the necessary equipment and personnel, needs to be in place to administer stem cell therapies safely and effectively.
The cost of stem cell therapies can pose challenges in terms of accessibility, particularly for individuals from lower-income backgrounds or regions with limited healthcare resources. It is essential to consider strategies to make these therapies more affordable and accessible to those who would benefit from them.

Clinical Trials and Research in Malaysia
Current Status of Stem Cell Research
Malaysia has made significant progress in stem cell research, including research related to AMD. Several institutions and research centers in the country are actively engaged in studying the potential of stem cell therapies for addressing various diseases and conditions, including AMD.
Clinical trials and studies are being conducted to assess the safety and efficacy of different stem cell-based approaches for treating AMD. These trials involve the transplantation of stem cells into the eyes of AMD patients and monitoring their effects on visual function and disease progression. The outcomes of these trials will provide valuable insights into the potential of stem cell therapies for AMD in the Malaysian context.
Potential Benefits for Malaysian Patients
The development of stem cell therapies for AMD in Malaysia holds several potential benefits for patients in the country. Firstly, it could offer a new treatment option for individuals with AMD who do not respond well to existing therapies or have limited access to them. Stem cell therapies have the potential to halt or reverse the progression of AMD, leading to improved vision and quality of life for patients.
Secondly, the development of stem cell therapies in Malaysia could contribute to advancements in healthcare and biomedical research in the country. Stem cell research requires collaboration between different disciplines and institutions, leading to the development of new technologies, discoveries, and expertise that can benefit the broader healthcare system.
Lastly, the availability of stem cell therapies for AMD in Malaysia could help reduce the burden on healthcare resources by offering a potential cure for the disease. By addressing the root causes of AMD and providing a long-lasting solution, stem cell therapies can reduce the need for ongoing treatments and interventions, leading to cost savings and improved healthcare efficiency.
International Progress and Success Stories
Breakthroughs in Stem Cell Therapies
Stem cell research has yielded several breakthroughs in the field of regenerative medicine, including the development of therapies for various diseases and conditions. In the context of AMD, there have been notable advancements in the use of stem cells to treat the disease.
One success story in stem cell therapies for AMD involves the use of human embryonic stem cell-derived RPE cells. In a clinical trial conducted in the United States, these cells were transplanted into the eyes of patients with advanced AMD. The results showed that the transplanted cells integrated into the retinal tissue and improved visual function in some patients.
Another breakthrough in stem cell therapies for AMD involves the use of iPSCs. Researchers have successfully reprogrammed adult cells, such as skin cells, into iPSCs and differentiated them into retinal cells, including RPE cells. Preclinical studies have shown promising results, with iPSC-derived RPE cells improving vision in animal models of AMD.
Clinical Trials and Results from Other Countries
Stem cell therapies for AMD have been the subject of clinical trials and research studies in various countries, including the United States, Japan, and the United Kingdom. These trials have evaluated different stem cell-based approaches, including the transplantation of stem cells into the eyes of AMD patients.
In Japan, a clinical trial using iPSC-derived RPE cells for the treatment of AMD is currently underway. The trial involves transplanting these cells into the eyes of patients with advanced AMD and monitoring their safety and efficacy over time. Early results from this trial have shown promising outcomes, with improvements in visual acuity and a reduction in the size of retinal lesions.
In the United States, the Food and Drug Administration (FDA) has granted several regenerative medicine advanced therapy (RMAT) designations for stem cell therapies targeting AMD. These designations recognize the potential of these therapies to address significant unmet medical needs and expedite their development and approval process.
These international clinical trials and research studies contribute to our understanding of the potential of stem cell therapies for AMD and pave the way for future advancements in the field.

The Future of Stem Cell Therapies
Potential for Personalized Medicine
One of the exciting prospects of stem cell therapies is their potential for personalized medicine. As mentioned earlier, iPSCs can be generated from a patient’s own cells, allowing for the development of personalized stem cell therapies. By using a patient’s own stem cells, the risk of rejection or immune response is minimized, increasing the safety and effectiveness of the treatment.
Personalized stem cell therapies for AMD could revolutionize the field by providing individualized treatments tailored to each patient’s specific needs and disease characteristics. This approach has the potential to improve treatment outcomes and reduce the risk of complications, leading to better quality of life for patients.
Collaboration and Knowledge Sharing
The development of stem cell therapies for AMD requires collaboration and knowledge sharing among different stakeholders, including researchers, clinicians, regulatory bodies, and industry partners. Collaboration allows for the exchange of ideas, expertise, and resources, leading to faster progress and more successful outcomes.
International collaborations and partnerships can facilitate the translation of research findings into clinical applications and ensure that the benefits of stem cell therapies are accessible to patients worldwide. By sharing knowledge and best practices, researchers and clinicians can learn from each other’s experiences and accelerate the development and implementation of stem cell therapies for AMD.
Overcoming Challenges and Expanding Access
While there are challenges and limitations in the development and implementation of stem cell therapies for AMD, efforts are being made to overcome these obstacles and expand access to these treatments.
Ongoing research and clinical trials aim to address the safety and efficacy concerns associated with stem cell therapies and provide the necessary evidence to support their use in clinical practice. Regulatory bodies play a crucial role in ensuring the quality and safety of these therapies, while also facilitating their timely approval and accessibility to patients who can benefit from them.
In terms of cost and accessibility, efforts are being made to reduce the financial burden associated with stem cell therapies and make them more widely available. These include initiatives to develop more cost-effective manufacturing processes, establish stem cell banking services, and explore alternative funding models to support the development and commercialization of these therapies.
By addressing these challenges and expanding access to stem cell therapies, it is possible to improve the outcomes for individuals with AMD and pave the way for a future where vision loss due to this debilitating condition can be effectively prevented or treated.
Conclusion
Age-related macular degeneration is a significant public health concern in Malaysia, with a high prevalence among the aging population. Traditional treatment options have limitations and do not provide a complete solution for addressing the root causes of the disease. However, the field of stem cell therapies offers new hope for individuals with AMD by providing the potential to restore vision and improve quality of life.
Through advancements in stem cell research, including the use of induced pluripotent stem cells, embryonic stem cells, and adult stem cells, it is possible to develop personalized and effective therapies for AMD. Clinical trials and research studies in Malaysia and other countries have shown promising results, paving the way for future advancements in the field.
While there are challenges and limitations to be addressed, through collaboration, knowledge sharing, and overcoming obstacles related to safety, regulatory frameworks, ethics, and accessibility, stem cell therapies for AMD can be made more widely available and contribute to significant improvements in the lives of patients.
The future of stem cell therapies holds the potential for personalized medicine, where individualized treatments based on a patient’s specific needs and characteristics can be developed. By harnessing the power of stem cells and working together to overcome challenges, it is possible to envision a future where age-related macular degeneration is effectively preventable and treatable, preserving vision and enhancing the quality of life for millions of individuals in Malaysia and beyond.